Sciatica is one of the most common—and most misunderstood—causes of lower back and leg pain. While it can feel severe and alarming, most people recover without surgery when the condition is managed correctly.
This pillar guide brings together current clinical evidence, recovery-focused guidance, tables, and data-backed visuals to help readers understand what sciatica is, what actually works, and how to prevent it from coming back.
Table of Contents
What Is Sciatica?
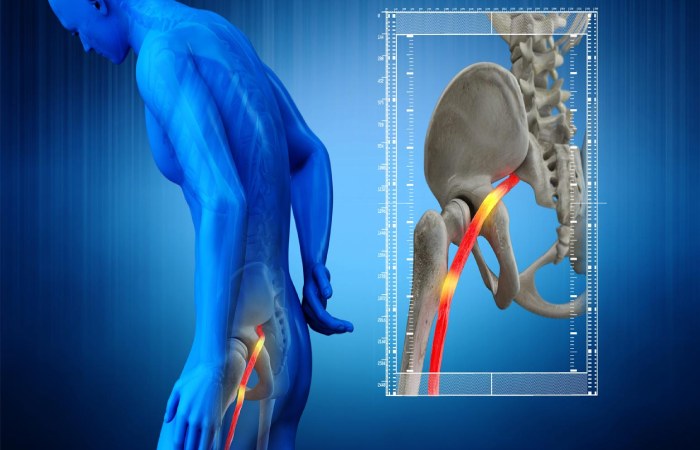
Sciatica is nerve pain from an injury or irritation to your sciatic nerve. In addition to pain, it can involve tingling or numbness in your back or butt that may also radiate down your leg. More severe symptoms are also possible.
Your sciatic nerve is the longest and thickest nerve in your body. It’s up to 2 centimeters wide (a U.S. penny or a United Kingdom 1 pence coin are about the same width). Despite its name, it’s not just one nerve. It’s actually a bundle of nerves that come from five nerve roots branching off from your spinal cord.
You have two sciatic nerves, one on each side of your body. Each sciatic nerve runs through your hip and buttock on one side. They each go down the leg on their side of your body until they reach just below your knee. Once there, they split into other nerves that connect to parts farther down, including your lower leg, foot and toes.
Having sciatica means you can experience mild to severe pain anywhere with nerves that connect to the sciatic nerve. The symptoms can affect your lower back, hips, buttocks or legs. Some symptoms may extend as far down as your feet and toes, depending on the specific nerve(s) affected.
Common Symptoms of Sciatica
- Pain worsened by prolonged sitting
- Muscle weakness or heaviness in the affected leg
- Sharp, shooting, or burning pain radiating down one leg
- Tingling or numbness in the leg or foot
Red‑Flag Symptoms (Seek Immediate Care)
- Progressive leg weakness
- Foot drop
- Loss of bladder or bowel control
What Causes Sciatica?
While disc herniation is the most well‑known cause, sciatica usually results from a combination of structural and lifestyle factors.
Primary Causes & Risk Factors
| Cause / Risk Factor | Contribution Level | Clinical Notes |
| Lumbar disc herniation | High (~90%) | Most common cause |
| Sedentary lifestyle | Moderate–High | Increases disc pressure |
| Obesity | Moderate | Raises recurrence risk |
| Smoking | Moderate | Slows disc healing |
| Genetic disc degeneration | High | Often overlooked |
What are the complications of sciatica?
Most people recover fully from sciatica. However, a possible complication of sciatica is chronic (long-term) pain.
If there’s serious damage to an affected nerve, chronic muscle weakness, such as a “drop foot,” might happen. That’s when nerve damage causes numbness in your foot, which makes normal walking difficult or even impossible.
Sciatica can also potentially cause permanent nerve damage, resulting in a loss of feeling in the affected legs.
How Sciatica Is Diagnosed
A healthcare provider can diagnose sciatica using a combination of methods. They’ll review your medical history and ask about your symptoms. They’ll also do a physical examination. That exam will include:
Walking. Sciatica often causes visible changes in how you walk. Your provider will watch for those changes as part of diagnosing sciatica.
Straight leg raise test. This involves having you lie on an exam table with your legs straight out. They’ll slowly raise your legs one at a time toward the ceiling and ask when you start to feel pain or other symptoms. These can help pinpoint the cause of sciatica and how to manage it.
Other flexibility and strength checks. These can help your provider determine if any other factors are causing or contributing to your sciatica.
Sciatica is primarily a clinical diagnosis based on:
- Symptom pattern
- Neurological exam
- Straight‑leg raise test
Imaging (MRI/CT) Is Recommended Only When:
- Symptoms persist beyond 6–8 weeks
- Significant weakness is present
- Surgery is being considered
Early imaging often finds abnormalities that do not correlate with pain, which can increase fear without improving outcomes.
Evidence‑Based Treatments Ranked by Effectiveness
Most sciatica cases improve with conservative care. The key is choosing treatments supported by evidence—not trends.
Treatment Comparison Table
| Treatment Option | Effectiveness | Evidence Strength | Recovery Impact |
| Physical therapy | High | Strong | Reduces recurrence ~50% |
| Progressive activity | High | Strong | Faster functional recovery |
| NSAIDs | Moderate | Moderate | Short‑term pain relief |
| Steroid injections | Moderate | Short‑term | Temporary symptom relief |
| Surgery (selected cases) | High | Strong | Faster pain relief, similar long‑term outcomes |
What Slows Recovery (Common Mistakes)
- Prolonged bed rest
- Avoiding all movement due to fear
- Returning to heavy activity too quickly
- Relying only on pain relief without rehabilitation
Recovery depends more on restoring movement tolerance than eliminating pain immediately.
Typical Recovery Expectations
| Type of Sciatica | Initial Improvement | Expected Full Recovery |
| Acute sciatica | 2–6 weeks | 6–12 weeks |
| Sub‑acute sciatica | 6–12 weeks | 3–6 months |
| Chronic sciatica | Gradual | Variable (needs rehab) |
Top Sciatica / Spine Specialists – USA vs India (2026)
| Country | Specialist Name | Specialty / Focus | Location / Affiliation |
| USA | Dr. John Rhee, MD | Orthopedic spine surgeon – complex lumbar/cervical conditions including sciatica | Los Angeles, CA – Emory Healthcare / Cedars-Sinai affiliation (spine care) |
| USA | Dr. Scott Boden, MD | Orthopedics & spine specialist – spinal fusion and degenerative spine disorders | Atlanta, GA – Emory Orthopaedics & Spine Center |
| USA | Dr. Robert S. Biscup, DO | Orthopaedic surgeon – minimally invasive spinal surgery & disc herniation | Cleveland Clinic Florida / Spine care programs |
| USA | Dr. John V. Prunskis | Interventional pain management and spine specialist – sciatica & chronic pain | Colorado & Illinois (Pain and Spine care) |
| USA | Dr. Kevin Pauza | Physiatrist & interventional spine specialist – disc regeneration therapies | Tyler, TX – Texas Spine and Joint Hospital |
| USA | Dr. Toure Barksdale, MD | Physiatrist / rehabilitation specialist – sciatica and lumbar radiculopathy | Rochester, MN – Specialty rehabilitation clinic |
| India | Dr. Ashish Dagar | Orthopaedic & spine specialist – sciatica / spinal conditions | Multiple cities (India) – highly rated clinician |
| India | Dr. Hitesh Garg | Orthopaedic spine surgeon – minimally invasive / complex spine pathology | Artemis Hospital, Gurugram |
| India | Dr. Karthik N. Vishwanathan | Advanced specialist – sciatica & herniated disc treatment | Vadodara (India) – MediFind advanced category |
| India | Dr. Satishchandra K. Gore | Advanced sciatica specialist – nerve pain / decompression surgery | Jintur (India) – MediFind recognized specialist |
| India | Dr. Rajkiran R. Banala | Advanced expert – sciatica and spine surgeries | Secunderabad (India) – MediFind listings |
| India | Prof. (Col.) Dr. Bipin Walia | Spine surgeon – trauma & spine care | India – known for spine and trauma expertise |
| India | Dr. V. Selvin Prabhakar | Spine surgeon – sciatica / disc surgery | Chennai (India) – expert spine surgeon |
When Is Surgery Really Necessary?
Surgery is appropriate for a small percentage of patients (5–10%).
Clear Indications
- Progressive neurological deficit
- Cauda equina syndrome
- Severe pain persisting after adequate conservative care
Long‑term outcomes for surgery and non‑surgical care are often similar, making proper patient selection essential.
Preventing Sciatica From Coming Back
Evidence‑based prevention focuses on capacity, not avoidance:
- Daily walking (30 minutes or more)
- Core and hip strengthening
- Gradual load progression
- Weight management
- Smoking cessation
- Regular breaks from prolonged sitting
Structured prevention programs can cut recurrence risk nearly in half.
Key Takeaways
- Sciatica is common but rarely dangerous
- Most people recover without surgery
- Movement and education outperform rest
- Long‑term success depends on rebuilding strength and confidence
Frequently Asked Questions (FAQs)
What is the main cause of sciatica?
The most common cause of sciatica is a lumbar disc herniation, which accounts for roughly 90% of cases. Other causes include spinal stenosis, degenerative disc changes, and lifestyle factors such as prolonged sitting and obesity.
How long does sciatica usually last?
Acute sciatica often improves within 2–6 weeks, with full recovery in 6–12 weeks. Sub-acute or chronic sciatica may take longer and usually requires structured rehabilitation.
Will sciatica go away on its own?
Yes. About 80–90% of people recover without operation, especially when they stay active, follow evidence-based exercises, and avoid prolonged bed rest.
What is the best treatment for sciatica?
The most effective treatments are physical therapy, progressive movement, and patient education. Medications and injections may help temporarily, but long-term recovery depends on restoring strength and movement tolerance.
When should I see a doctor for sciatica?
You should seek medical care if pain is severe or worsening after several weeks, or immediately if you experience progressive leg weakness, numbness in the groin area, or loss of bladder or bowel control.
Does sciatica require surgery?
Only 5–10% of patients require operation. It is usually recommended when there is significant nerve damage, worsening weakness, or persistent pain that does not respond to conservative treatment.
Is walking Good for sciatica?
Yes. Gentle walking is one of the safest and most effective activities for sciatica, as it supports circulation, reduces stiffness, and supports recovery without overloading the spine.
Can sciatica come back after recovery?
Yes, sciatica can recur, especially without proper rehabilitation. However, exercise-based prevention programs can reduce recurrence risk by nearly 50%.
